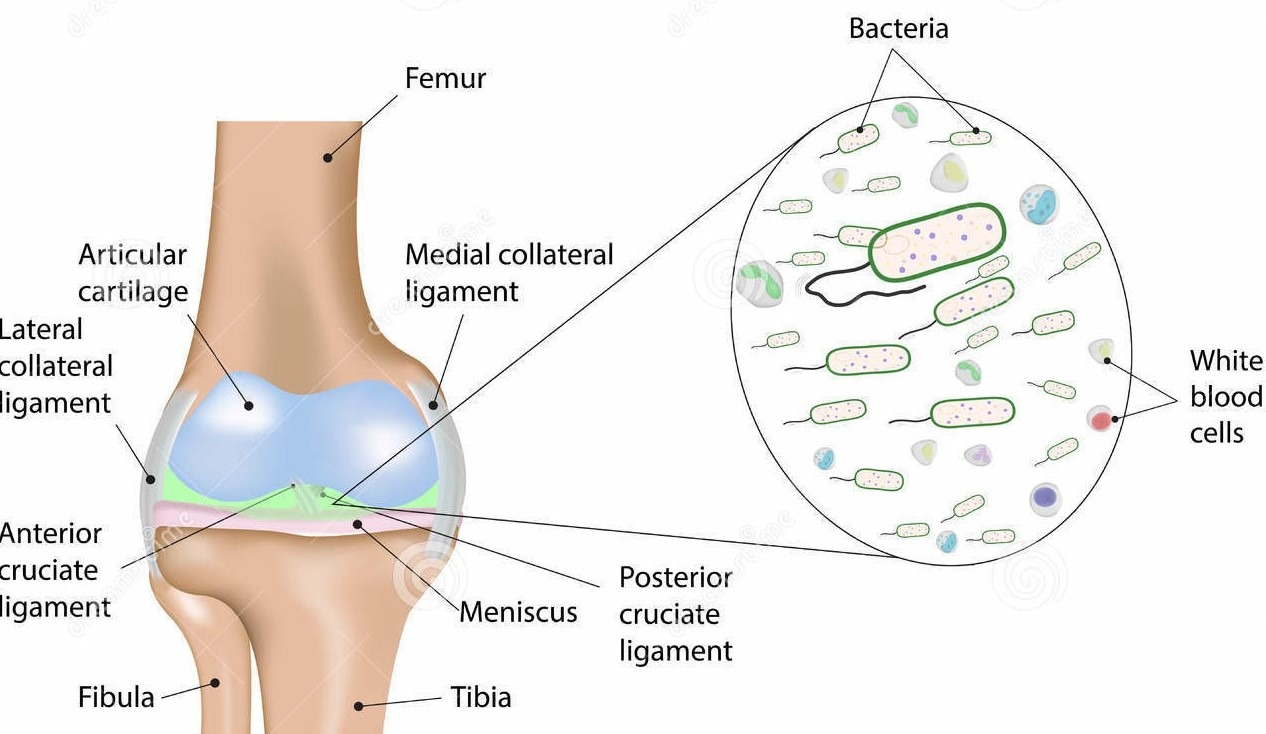
A joint that becomes inflamed as a result of an infection is said to be septic. Damage to the joint surface, or cartilage, as a result of infection is termed septic arthritis.
What are the causes?
Bacteria may enter a joint through a break in the skin, through the bloodstream from another source of infection, or as a result of an injection or surgery. Some joint infections occur without any known cause. People whose immune systems are impaired are at increased risk for septic joints.
What are the symptoms?
Patients with septic joints complain of pain and swelling in the joint. The joint is hot, red, and extremely painful to bear weight. Range of motion of the joint is greatly reduced. The joint is swollen and tender to the touch. Patients may have a fever.
How is it diagnosed?
Dr. Chandrasekaran will diagnose a septic joint on clinical exam. Laboratory studies may show an elevated white blood cell count, and tests for inflammation such as ESR and CRP will be elevated. Fluid drawn from the affected joint will be purulent and can be analyzed for bacteria and white blood cells. X-rays and an MRI may show fluid in the joint.
How it is treated?
Non-Operative
Because a bacterial infection in a joint is damaging to cartilage, septic joints are considered to be relative surgical emergencies. Non-operative treatment, consisting of antibiotics and draining the joint several times with a needle and syringe, is reserved only for patients too sick to undergo an operation.
Operative
Dr. Chandrasekaran will wash the joint in the operating room, either arthroscopically or through an open incision to remove the bacteria. Cultures will be taken from inside the joint to identify the type of bacteria responsible. Intravenous antibiotics will be given to help eradicate the infection. Blood tests will confirm that the infection has resolved.